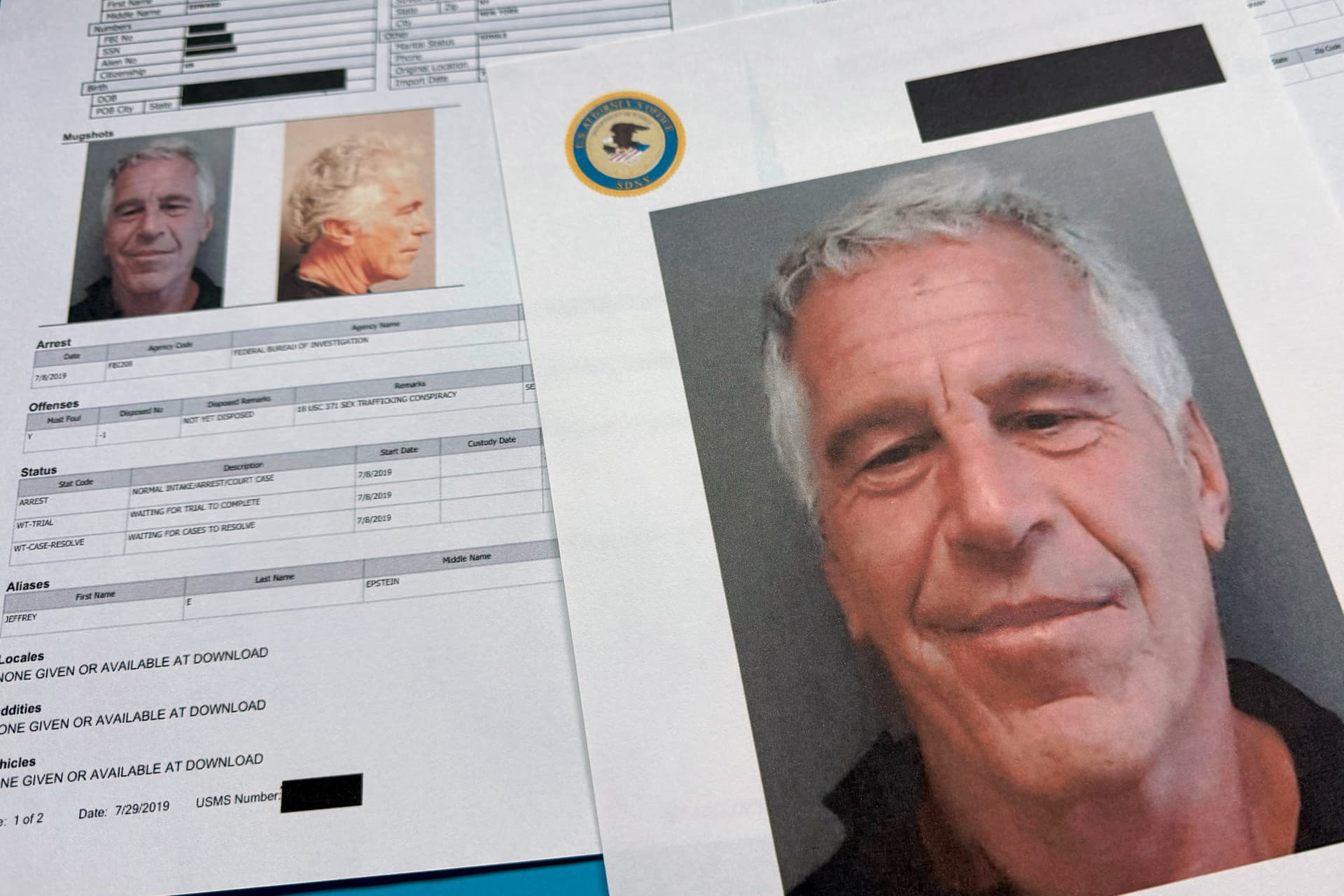
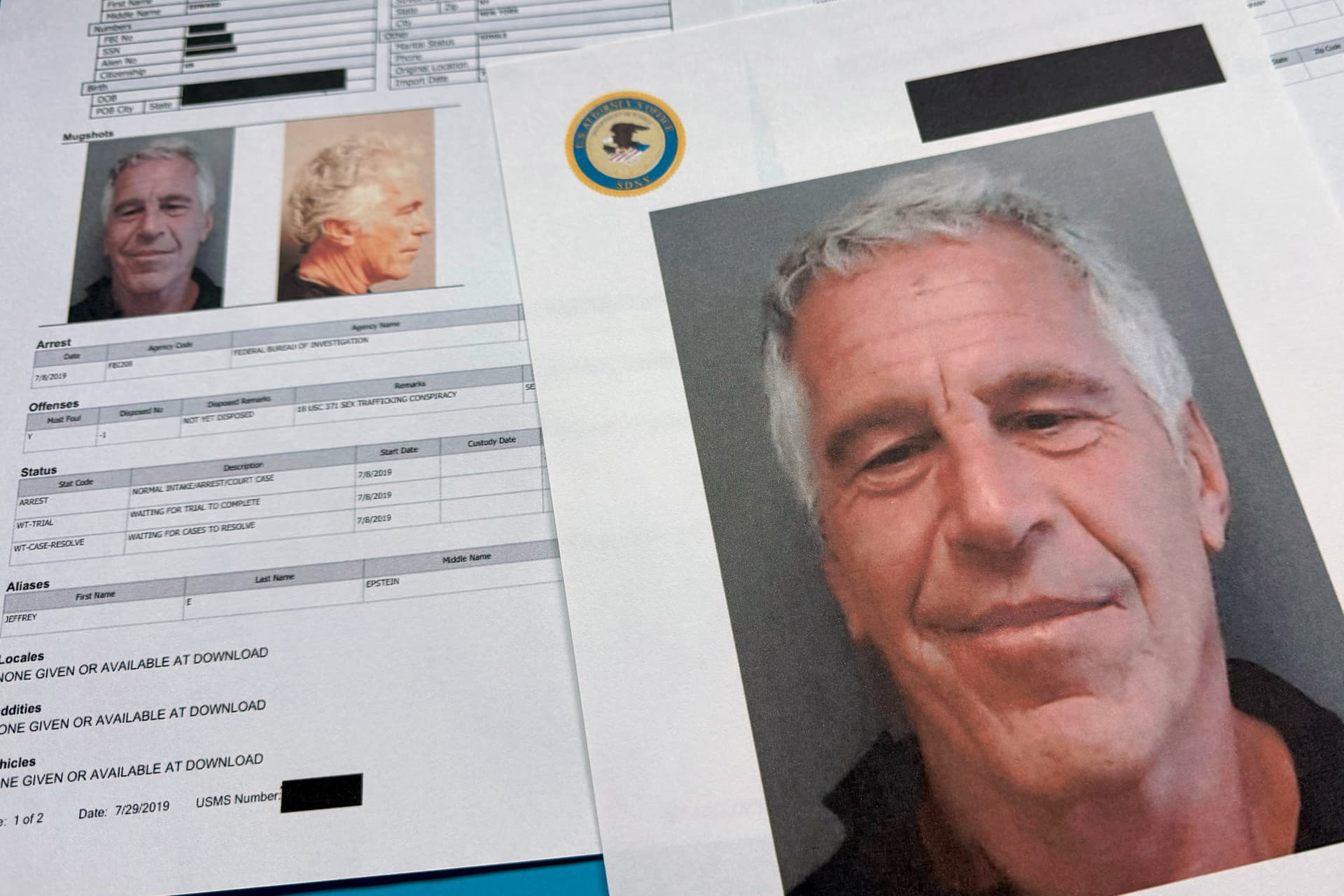
Final Release of Epstein Files Details Ties to Tech Titans and Top Officials but Fails To Satisfy Critics
By JOSEPH CURL
|This article is from the archive of The New York Sun before the launch of its new website in 2022. The Sun has neither altered nor updated such articles but will seek to correct any errors, mis-categorizations or other problems introduced during transfer.

Already have a subscription? Sign in to continue reading
$0.01/day for 60 days
Cancel anytime
By continuing you agree to our Privacy Policy and Terms of Service.
By JOSEPH CURL
|
By JAMES BROOKE
|
By CAROLINE McCAUGHEY
|
By LUKE FUNK
|
By A.R. HOFFMAN
|
By NOVI ZHUKOVSKY
|
By SALENA ZITO
|
By MICHAEL BARONE
|